Step-by-Step: What You Need to Know About HbA1c
HbA1c Is Not a Blood Sugar Test
HbA1c is a glucose exposure log of your red blood cells (RBCs). It reflects how much glucose sticks to your hemoglobin over time. Two major factors affect this:
| Variable | Represents |
|---|---|
| Blood Glucose | How much sugar is circulating in your blood |
| RBC Lifespan | How long red blood cells remain in circulation |
What this means: A shorter lifespan of RBCs leads to a skewed (higher) HbA1c—even if your actual blood sugar levels are stable.
Hard Training Alters RBC Biology
High-volume, mixed-modality training causes:
-
Mechanical trauma (foot-strike hemolysis)
-
Oxidative stress
-
Elevated erythropoietin (EPO) levels
-
Faster RBC turnover
This results in:
-
Younger, more permeable RBCs
-
Increased glucose binding to hemoglobin, even with normal blood glucose levels
-
Shortened RBC lifespan, which disrupts the A1c average
This is not dysfunction—it’s adaptation. Your body is regenerating red cells quickly to meet the oxygen and metabolic demands of training.
You Could Be Misrepresented by Proxy
An elevated A1c might look like poor glycemic control, but in active individuals, it often reflects:
-
Enhanced RBC turnover (not chronic hyperglycemia)
-
Hemoglobin variants
-
Subclinical oxidative stress
The result? A potential clinical red flag that doesn’t match your physiological reality.

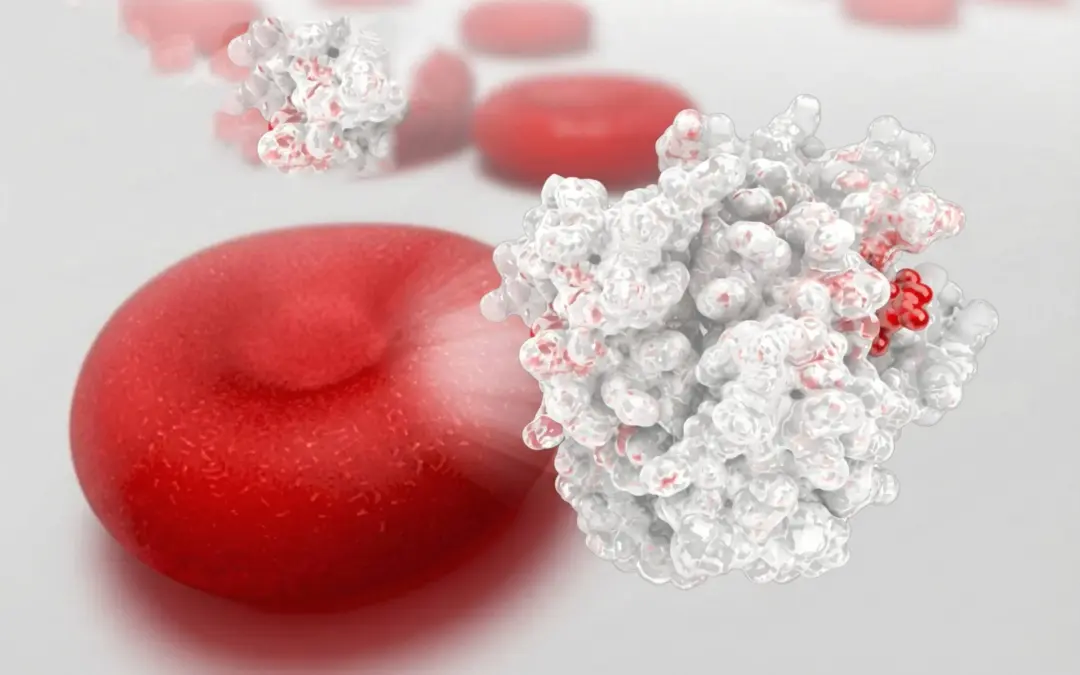
Core Concepts: Systems vs Snapshots
HbA1c is a static snapshot. Your body is a dynamic system.
Physiology doesn’t happen in isolated events—it unfolds as a symphony of integrated adaptations across respiratory, cardiovascular, neuromuscular, and cellular systems. Measurements that fail to account for this complexity could be incomplete or misleading.
This becomes more important when we recognize the core truth of Fluid Health’s philosophy:
Structure precedes conditioning. Movement quality precedes intensity.
Misinterpreting data often leads people to reactive behaviors—over-correcting nutrition, under-fueling training, or even fearing exercise—when the actual need is to better understand why these biomarkers behave differently in trained systems.
Preparation: What to Do Before Your Next Blood Test
To better interpret your metabolic health, preparation matters:
Pair A1c with other data points: Include fasting glucose, insulin, fructosamine, and continuous glucose monitor (CGM) trends if possible.
Document training load: Especially 7-10 days prior to testing.
Track subjective metrics: Sleep quality, energy, recovery, mood.
Know your baseline: If you have previous labs when untrained, compare those to now.
How to Take Action
(Without Overreacting)
Once your labs are in, use this structured approach:
1. Contextualize the Data
Ask: Does this result make sense given my training, nutrition, recovery, and current stress load?
If the answer is yes, don’t jump to pathology.
2. Engage with Clinicians Who Understand Active Physiology
Share your training history and request an interpretation that accounts for:
-
Elevated RBC turnover
-
Shifts in mitochondrial function
-
Training-induced oxidative adaptation
3. Focus on Functional Markers
These include:
-
Resting heart rate and heart rate variability (HRV)
-
Metabolic testing results (RER, VO2 max, lactate threshold)
-
Movement assessments (e.g., DNS, PRI, postural restoration)
4. Avoid Overcorrecting
Don’t:
-
Eliminate carbohydrates unnecessarily
-
Increase stress by over-fasting or under-eating
-
Reduce training intensity without cause
Why This Perspective Heals
If you’re the type of person drawn to structured movement and data-driven outcomes, you’re also likely someone who wants control over your health narrative.
When a misunderstood lab derails your confidence, it does more than disrupt your training—it misaligns your identity.
By reframing HbA1c through a biomechanical, cellular, and respiratory systems lens, you restore autonomy. You see yourself not as broken, but as adaptive. As someone whose body reflects capacity—not chaos.
This mindset shift supports progressive behavior change:
| Stage | Reframe |
|---|---|
| Contemplation | “Maybe my body isn’t failing—I need better data.” |
| Preparation | “I’ll discuss this with an informed provider.” |
| Action | “I’ll retest with context and interpret wisely.” |
| Maintenance | “I trust my body’s signals and know how to respond.” |
Redefining Metrics for the Resilient
In clinical models, health is often reduced to numbers.
But you are not a number. You are a system in motion, shaped by intelligent stress and structural progression.
So next time an elevated HbA1c shows up on your labs, don’t panic.
Pause. Contextualize. And act from a place of understanding—not fear.
Because if you’re training hard, recovering well, and building structure before conditioning, your metrics may be “off”— but your health is likely right on track.

Medical & Educational Disclaimer